A collaborative study led by the Department of Physiology, Anatomy, and Genetics (DPAG), with Fellow in Physiology Professor Peter Robbins as the lead author, studied patients at six and twelve months after a COVID-19 infection, finding that prior COVID-19 infection was associated with more uneven inflation of the lungs during normal breathing. There was also an association between hospitalisation with COVID-19 and smaller lung volumes, and admission to the intensive care unit (ICU) was associated with an enlarged respiratory dead space.
As a respiratory disease, COVID-19 infection mainly affects the lungs. While most people recover completely, a significant number of individuals experience symptoms that can persist for weeks or months post-COVID infection, sometimes referred to as ‘long-COVID’. It remains unclear whether these symptoms are associated with any long-term damage that reduces the function of the lungs and respiratory system.
To investigate this, the study used a novel computational approach to assess how COVID-19 may affect long-term lung function. The results have been published in the Journal of Applied Physiology.
Key findings:
Prior COVID-19 infection was associated with more uneven inflation of the lungs during normal breathing. This is something that is part of normal ageing in the lung. The changes seen after COVID-19 in this study are roughly equivalent to those associated with 15 years of normal ageing, but are still much smaller than those seen in established lung disease.
There was an association between hospitalisation with COVID-19 and smaller lung volumes, but it is not known whether the smaller volumes are caused by COVID-19 infection, or instead represent a predisposing factor for more severe infection.
Admission to the ICU was associated with an enlarged respiratory dead space (the volume of gas that is breathed into the lungs but does not participate in gas exchange). This may have been caused by COVID-19 infection, but equally may have been caused by the process of mechanical ventilation.
The research team assessed lung function using a novel technique called computed cardiopulmonography. In this method, participants breathe through a mouthpiece connected to the measuring device that uses lasers to take highly precise measurements of gas composition. These measurements are then fed into a computational model of the respiratory and cardiovascular systems to estimate values for aspects relating to the individual’s lung function. For each individual, the model was adjusted to take into account physiological factors that can influence lung function, such as sex, age, height, and body mass.
This technique has already been shown capable of predicting whether patients with asthma required an increase in their medication. It also shows promise as a method to detect sub-clinical lung disease, opening the possibility of eventually treating patients earlier to prevent the onset of more significant disease.
Our study illustrates the capability of this new technique to study aspects of lung function not so easily measured through standard clinical tests. However, without measurements prior to infection, it is not possible to conclude whether these differences result directly from COVID-19 infection, or whether they are actual risk factors associated with the lungs that predispose towards more serious disease.
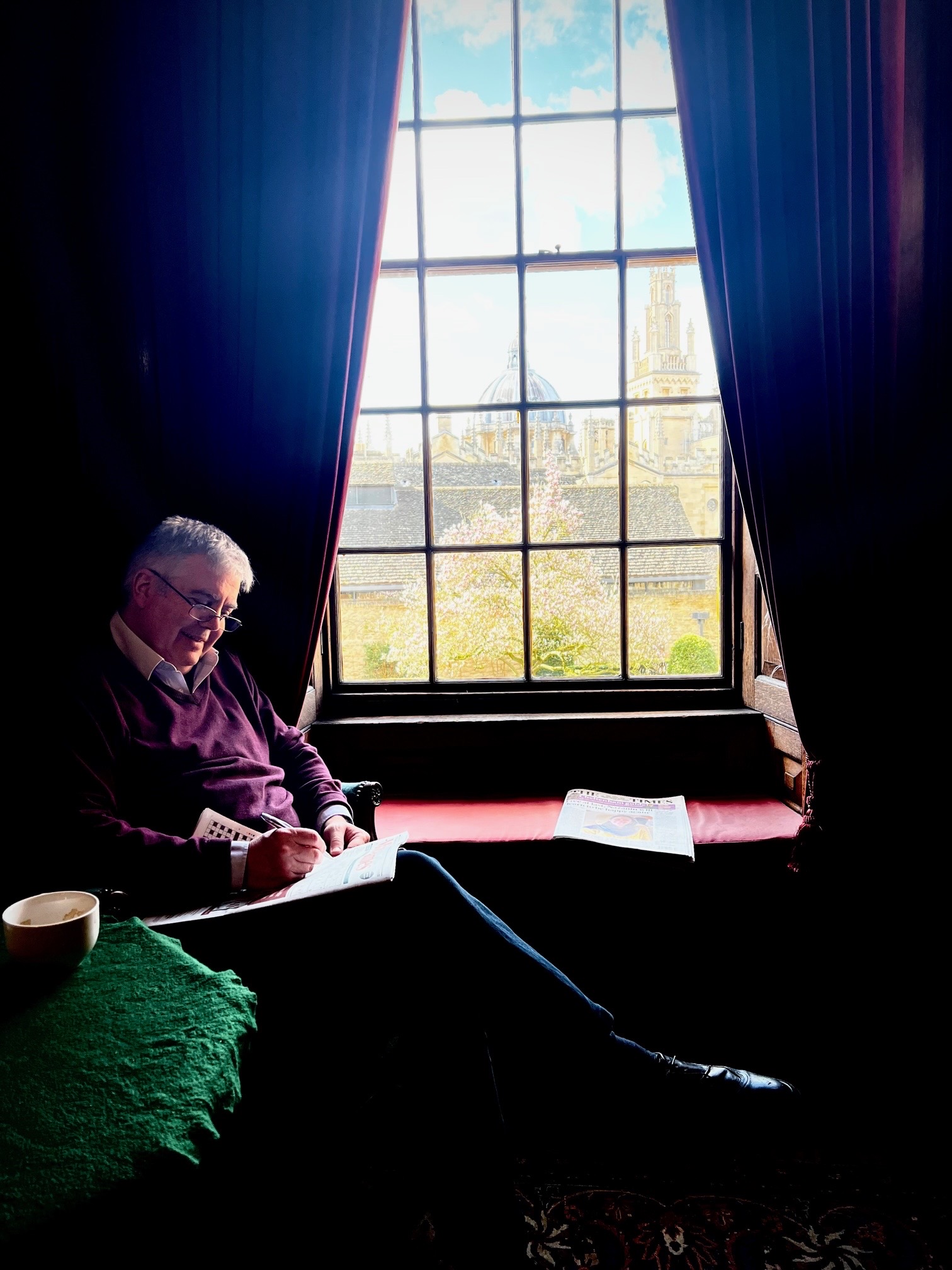
Lead author, and Fellow in Physiology at Queen’s, Professor Peter Robbins
The authors of the study would like to thank all the participants from the two cohorts who took part in the study. One cohort was comprised of members of the armed forces and was supported by the Defence Medical Services Group. The other cohort was recruited from the Oxford University Hospitals (OUH) post-COVID respiratory clinics and supported by a OUH Research Capability Fund and the University of Oxford’s COVID-19 Research Response Fund. Respiratory Consultant Dr Nayia Petousi, from the University of Oxford’s Nuffield Department of Medicine, and one of the clinical leads for the study, said: ‘We hope that by providing insight into the understanding of post-COVID effects on the lungs the results can be of help in the clinical management of patients.’
The novel technique used to make the measurements in this study is known as computed cardiopulmonography, and was developed with support provided by the National Institute of Health Research (NIHR) Oxford Biomedical Research Centre (BRC).
The paper was also authored by DPAG graduate students Snapper Magor-Elliott, Queen’s graduate student Asma Alamoudi, Haopeng Xu, Tishan Wellalagodage, alongside Departmental Lecturer and Consultant in Respiratory Medicine Dr Nick Talbot.