Professor of Molecular and Population Genetics Simon Leedham and his team have been awarded over £2m from Cancer Research UK to develop a new tool which could help guide how patients with bowel cancer are treated. We asked Professor Leedham to tell us more about his work and the impact of this funding.
Many congratulations on receiving the grant. What will it mean for the work that you and your team are doing?
This programmatic funding will allow my team and I to progress our research into colorectal cancer stem cells for the next five years. This level of support is necessary to allow fundamental research to develop and fully explore the exciting ideas we have to help colorectal cancer patients in the future.
Can you tell us a bit about how the new tool will help bowel cancer sufferers?
One of the key problems with treating cancer is the development of drug resistance. This problem arises because cancer is able to evolve in real time, and cancer cells have the capacity to adapt, when they are exposed to chemotherapy. Whilst some cells will be killed, other cells within the tumour survive and can change their behaviour and appearance – a leopard that can change its spots! This is known as cell plasticity. Using biological models we have shown that we can measure cell plasticity at a molecular level, following application of a selective pressure in tumours. We believe that we can use our stem cell molecular phenotyping tool to measure tumour cell behaviour following treatments and use this information to guide which therapies work best in which patient.
Why is it particularly effective to study cancers on the molecular level and how does it differ from other forms of cancer research?
It is very important to be able to measure the impact of different therapies on cancers, that way we can assess which treatments are effective. In most tumours the current most useful way to assess tumour response is to undertake cross sectional imaging like CT, MRI or PET scan. This imaging can tell us a lot about tumour size and can even inform on the metabolic response to treatment, but cannot give us a detailed picture on what is happening at a cellular and molecular level. In colorectal cancer, tissue sampling is safe, painless, and comparatively easy, through the use of endoscopy which is a well-tolerated procedure. By undertaking repetitive sampling from tumours in colorectal cancer patients on treatments, we can undertake detailed molecular testing on tumours before and after therapy which will help us to decide which treatments to use, in which order, to maximise cancer cell killing.
What does a typical day in the lab look like for you?
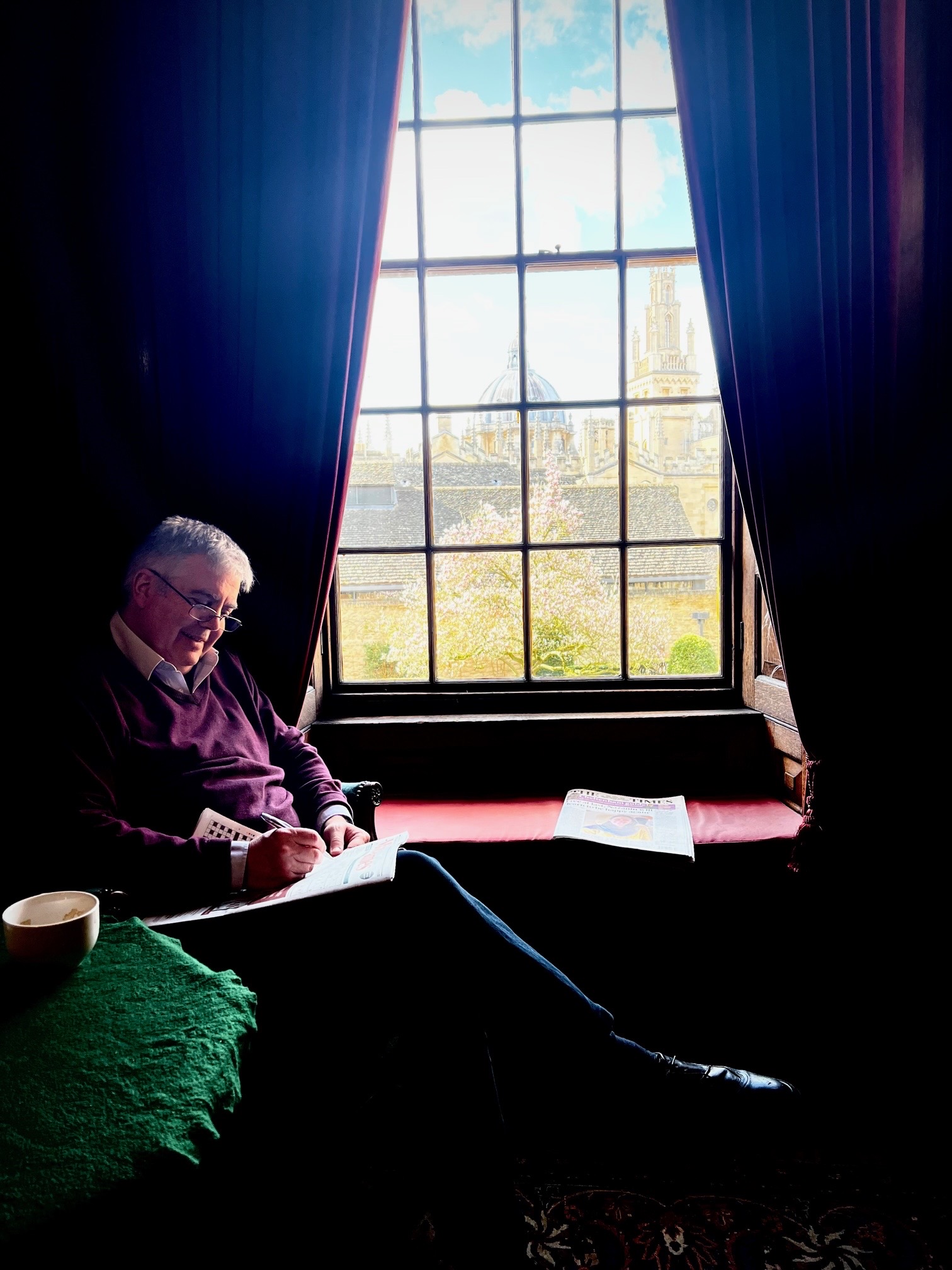
I’m lucky to work with a team of outstanding scientists, students, and collaborators so the best parts of my day are spent catching up on work and discussing new ideas with them. There is little more interesting and intellectually stimulating than a work-in-progress meeting with a dedicated colleague! As an academic PI (Principal Investigator) you are also the equivalent of a CEO of a small company so there are always plenty of financial and ethical administrative tasks, grant applications, and papers to write as well as stemming the daily flood of the e-mail river!
What’s the best thing about working in Oxford?
The people. I am privileged to be able to interact with international experts across a wide range of multidisciplinary fields, each bringing a new perspective on a shared problem.